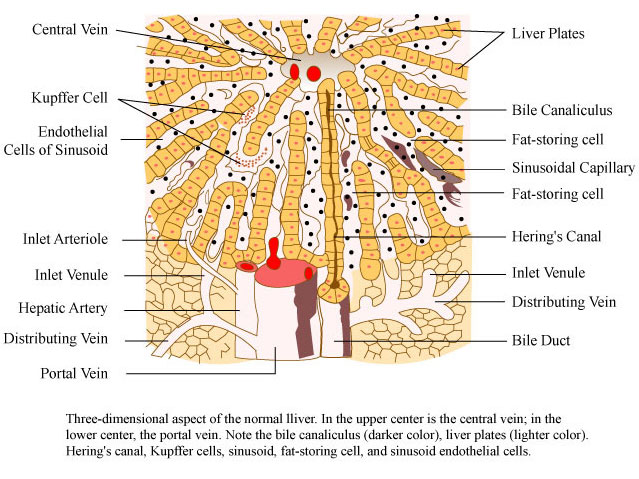
Hepatic parenchyma is the part of the liver that filters toxins from the blood. It is a biochemical laboratory, essentially, where several different processes are taking place:
- Bile production, responsible for fatty acids digestion
- Coagulator factors biosynthesis (vitamin K), responsible for clotting mechanisms
- Synthesis of the majority of proteins that circulate in the plasma, including albumin and most of the globulins
- Glycogen storage as energy supply (glycogenesis), breaking glycogen down to glucose (glycogenolysis) and forming glucose from noncarbohydrate sources (gluconeogenesis)
- Lipoproteins construction (HLD & LDL), responsible for atherogenesis -atheromatosis inflammatory processing in arterial endothelium
- Hormonal production (IGF1-somatomedin C)
- Vitamin storage (cyanocobalamin-B12)
- Cleansing and detoxifying of chemicals (paracetamol, nonsteroidal anti-inflammatory drugs-NSAID, glucocorticoids, alcohol-ethanol, anabolic-androgenic steroids-AAS).
Whenever a chemical substance enters the portal circulation and the liver afterwards, the liver has to detect either this is a toxic material, or something useful for the system. The liver metabolizes many drugs that do not cause liver strain. However, AAS can be responsible for a wide variety of types of clinical and hepatic strain, and injury to the organ. Biochemical markers such as the liver enzymes, known as transaminases (alanine transaminase -ALT/SGOT and aspartate transaminase-AST/SGPT), alkaline phosphatase (ALP), γ-glutamyl transpeptidase (GGT), lactate dehydrogenase (LDH) and bilirubin (Bil) are often used to indicate liver damage. Liver injury is defined as a rise in either:
- (a) ALT level more than three times of upper limit of normal,
- (b) ALP level more than twice upper limit of normal, or
- © total bilirubin level more than twice upper limit of normal, when associated with increased ALT or ALP. Liver damage is further characterized into hepatocellular (ALT elevation) and cholestatic (ALP rise) types.
AAS according to liver toxicity are classified into two main categories:
- (a) The 17-alkylated AAS (most of them are oral, tabs-per os),
- (b) The non 17-alkylated AAS (most of them injectables).
The only injectable 17-alkylated AAS is stanozolol (Winstrol Depot), while the only non 17-alkylated oral pills are:
- mesterolon (Proviron)
- methenolon (Primobolan acetate)
- testosterone undecaonate (Andriol).
The most potent 17 alkylated per os are:
- methyltrienolone (M3)
- fluoxymesterone (Halotestin)
- oxymetholone (Anadrol 50)
- methandrostenolone-methandienone (Dianabol)
- methyltestosterone (Teston)
- stanozolol (Winstrol)
- oxandrolone (Anavar).
All AAS are responsible for atheromatic index distortion, and shifting of the lipoproteins ratio (HDL/LDL). This eventually may lead to cardiovascular disease (CVD). Alkylation of the steroid molecule ensures that the particular substance will sustain any hostile environment, such as in gastric juice (acidic). When the substance enters the hepatic parenchyma, through circulation, the liver has to metabolize it. Alkylation is something hard to break, therefore this stresses hepatocytes. This may result in AST, ALT increasing their serum values (>100).
Injectable AAS and to some extent even injectable 17 alkylated AAS (stanozolol suspension) are less toxic for the liver. One reason is that the substance bypasses the portal-hepatic circulation and enters into the blood stream from intramuscular circulation (par enteric). This affects indirectly the liver, thus strain is less. Aside from stanozolol, injectable substances do not possess 17-alkylation. This makes them far easier for the liver to metabolize. A tricky method in order for 17 alkylated oral AAS to be less toxic is to be used sublingually, i.e. under the tongue. That specific area in the oral cavity is full of tiny blood vessels. Acute absorption occurs; therefore the steroid substance enters into the blood stream, as it had been administrated intramuscularly. In this way, the substance does not become as concentrated in the liver as after oral dosing, and less (but still significant) liver strain may occur.
AAS have been involved in four distinct forms of liver injury:
- Pharmaceutical hepatitis; in that case, liver transaminases are elevated (>100). These elevations are attributed to the intake of oral steroids, are usually asymptomatic, transient and return to baseline levels within several weeks after cessation. Such elevations have been most closely linked to fluoxymesterone and oxymethalone. Occasionally this is mis-diagnosed with muscle damage/rhabdomyolysis (CPK>500) rather than hepatic dysfunction, since both hepatocytes and muscle cells posses receptors for SGOT and SGPT enzymes. Recently, studies demonstrated that GGT is the most distinctive enzyme for the detection of hepatic dysfunction.
- Cholestasis; a condition where jaundice occurs. There is not proper elimination of bile, through bile duct and bile tubules intracellular of liver parenchyma. The onset is usually accompanied with development of nausea, fatigue and itching followed by dark-brownish urine (elevated urobilinogen) and jaundice (elevated bilirubin). Jaundice can be prolonged even if the AAS are discontinued. Typically, serum elevations of cholestatic markers such as ALP, γGT, bilirubin-direct/indirect, are present. Liver biopsy typically shows cholestasis with inflammation, hepatocellular necrosis and hyperplasia of hepatocytes. This clinical phenotype of cholestasis is typical of the use of AAS.
- Hepatic peliosis; is a rare syndrome in which liver lobes are covered with nodulation that contain blood cysts. The liver may be enlarged, deep red in color. Serum enzyme levels are usually normal or mildly elevated. Patients may present with right upper discomfort. This is a critical and sometimes fatal condition. However, peliosis associated with AAS usually reverses, at least in part, in case the patient discontinuates AAS abuse for good.
- Hepatocellular carcinoma; the most serious complication of AAS use is the development of hepatic tumors, either adenoma (HCA) or hepatocellular carcinoma (HCC). Clinical presentation is generally with right upper quadrant discomfort and a hepatic mass found clinically or on imaging studies (U/S,C/T). Routine liver tests are often normal, unless there is extensive spread or rupture or any accompanying liver disease. While fluoxymesterone is associated with HCA formation, other substances like oxymetholone, respectively, methyltestosterone can lead to HCC. There are different therapeutic strategies for HCC without metastasis. In general liver transplantation is the therapy of choice for selected patients with HCC without the possibility of extrahepatic metastasis. Abuse of AAS over a long period of time has a risk of developing an HCC and users should therefore be well monitored. Periodic hepatic ultrasound seems to be an adequate screening procedure to detect the development of hepatic lesions.
Fatty liver disease is a condition mainly due to metabolic reasons. Obesity and metabolic syndrome usually lead to fat accumulation within liver parenchyma. In some cases, fatty liver may be accompanied by hepatic inflammation and liver cell death (steatohepatitis). This case is reversible, with proper nutrition and supplementation of lipotropic factors (choline, inositol). Supplementation provides medical prevention and ensures that liver enzymes are not that much elevated. Ursodeoxycholic acid (UDCA) seems to be extremely useful in cases of cholestasis, where jaundice occurs. These bile salts have the ability to reduce bilirubin’s concentration, decrease the toxicity of the bile pool and reverse cholestatic evaluations (ALP, GGT).
Other powerful antioxidants, such as glutathione (injectable), or N-Acetyl-Cystein (N-A-C) are helpful as well. N-A-C is a glutathione’s precursor and serves as a liver detoxification agent. N-A-C serves to increase the glutathione reserves in the body and, together with glutathione; they both directly bind to toxic metabolites. Herbs as silimarin (milk thistle), or/and artichoke are known as being powerful antioxidants in the liver in particular. Alpha Lipoic Acid is also a potent agent against free radicals and oxidative stress. Taraxacum is a diuretic herb that cleanses and flushes away toxins through urine. There are several liver protecting formulas in the market. One of them is Liver Stabil by Molecular Nutrition. However, they have to be used with a diet low in SFA’s, and no alcohol or acetaminophen/paracetamol too. At least while the AAS user undergoes a steroid cycle.
References:
- Chitturi S, Farrell GC. Adverse effects of hormones and hormone antagonists on the liver. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 605-20. (Review of hepatotoxicity of androgenic steroids including cholestasis, vascular disorders, benign tumors and hepatocellular carcinoma).
- Mumoli N, Cei M, Cosimi A. “Drug-related hepatotoxicity”. N. Engl. J. Med. 2006; 354 (20): 2191–3
- Philipp Solbach, Andrej Potthoff, et al. Testosterone-receptor positive hepatocellular carcinoma in a 29-year old bodybuilder with a history of anabolic androgenic steroid abuse: a case report BMC Gastroenterol. 2015; 15: 60.
- Ursodeoxycholic acid and bile-acid mimetics as therapeutic agents for cholestatic liver diseases: an overview of their mechanisms of action. Poupon R. Clin Res Hepatol Gastroenterol. 2012 Sep; 36 Suppl 1:S3-12. doi: 10.1016/S2210-7401(12)70015-3.
image: Three dimensional aspect of the normal liver by MIT OCW.
By George Touliatos| September 15th, 2015